About us
Self-Care Week
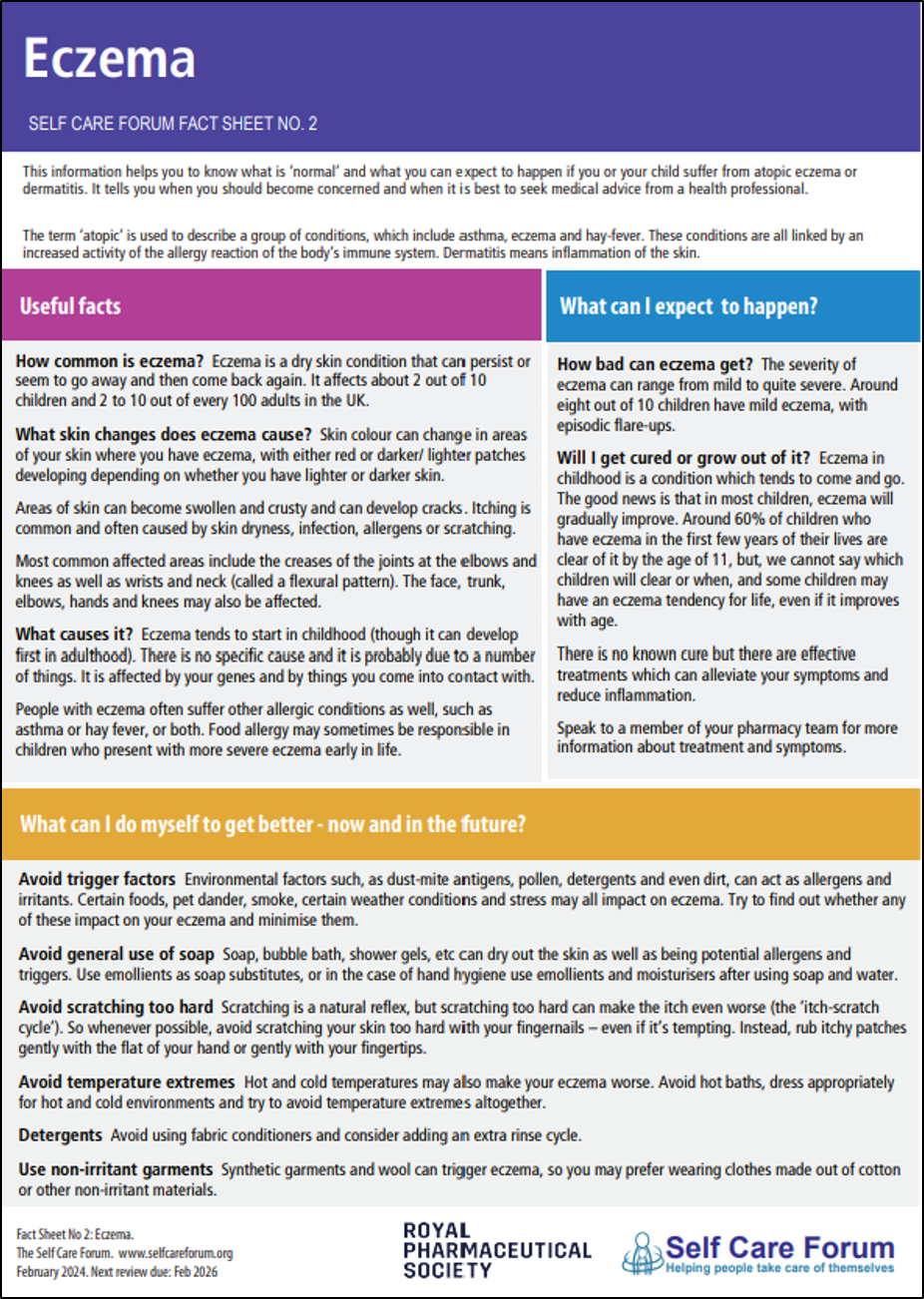
Factsheets
Resources