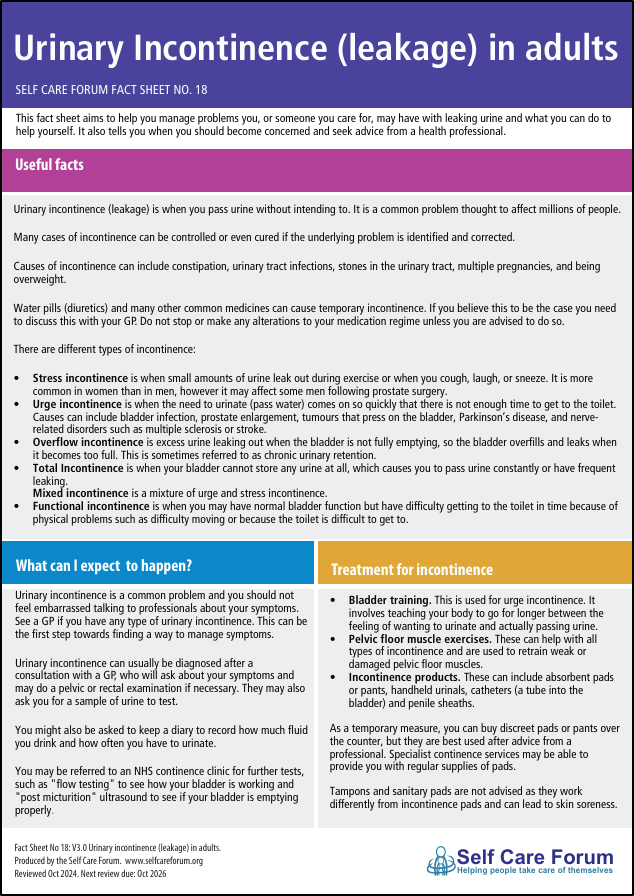
This page aims to help you manage problems you or someone you care for may have with leaking urine and what you can do to help yourself.
Useful facts
Urinary incontinence (leakage) is when you pass urine without intending to. It is a common problem thought to affect millions of people.
Many cases of incontinence can be controlled or even cured if the underlying problem is identified and corrected.
Causes of incontinence can include constipation, urinary tract infections, stones in the urinary tract, multiple pregnancies, and being overweight.
Water pills (diuretics) and many other common medicines can cause temporary incontinence. If you believe this to be the case you need to discuss this with your GP. Do not stop or make any alterations to your medication regime unless you are advised to do so.
There are different types of incontinence:
Stress incontinence is when small amounts of urine leak out during exercise or when you cough, laugh, or sneeze. It is more common in women than in men, however it may affect some men following prostate surgery.
Urge incontinence is when the need to urinate (pass water) comes on so quickly that there is not enough time to get to the toilet. Causes can include bladder infection, prostate enlargement, tumours that press on the bladder, Parkinson’s disease, and nerve-related disorders such as multiple sclerosis or stroke.
Overflow incontinence is excess urine leaking out when the bladder is not fully emptying, so the bladder overfills and leaks when it becomes too full. This is sometimes referred to as chronic urinary retention.
Total Incontinence is when your bladder cannot store any urine at all, which causes you to pass urine constantly or have frequent leaking.
Mixed incontinence is a mixture of urge and stress incontinence.
Functional incontinence is when you may have normal bladder function but have difficulty getting to the toilet in time because of physical problems such as difficulty moving or because the toilet is difficult to get to.
What can I expect to happen?
Urinary incontinence is a common problem and you should not feel embarrassed talking to professionals about your symptoms.
See a GP if you have any type of urinary incontinence. This can also be the first step towards finding a way to manage the problem.
Urinary incontinence can usually be diagnosed after a consultation with a GP, who will ask about your symptoms and may do a pelvic or rectal examination as appropriate. They may also ask you for a sample of urine to test.
The GP may ask you to keep a diary to record how much fluid you drink and how often you have to urinate.
You may also be referred to an NHS continence clinic where further tests may be performed. These may include flow testing to see how your bladder is working and ‘post micturition’ ultrasound to see if your bladder is emptying properly.
Non-Surgical Treatments
Bladder training. This is used for urge incontinence. It involves teaching your body to go for longer between the feeling of wanting to urinate and actually passing urine.
Pelvic floor muscle exercises. These can help with all types of incontinence and are used to retrain weak or damaged pelvic floor muscles.
Incontinence products. These can include absorbent pads or pants, handheld urinals, catheters (a tube into the bladder) and penile sheaths.
As a temporary measure, you can buy discreet pads or pants over the counter, but they are best used after advice from a professional. Specialist continence services may be able to provide you with regular supplies of pads. The Bladder and Bowel UK Charity website provides advice on managing incontinence.
Tampons and sanitary pads are not advised as they work differently from incontinence pads and can lead to skin soreness.
Medicines. Some medicines can help with specific types of incontinence. They include treatment for urge incontinence with ‘antimuscarinics’ such as oxybutinin and tolteradine, and mirabegron. Duloxetine, a medicine that is also used for depression and nerve problems is also licenced for use in women with stress incontinence.
Other non-surgical treatments
Other treatments you might be offered include electrical stimulation, biofeedback and vaginal cones (for women).
Surgery and other interventions
If non-surgical treatments have not worked or are not suitable, you may be referred for consideration of a surgical procedure.
These might include (and would be fully explained by your specialist):
For stress incontinence
Colposuspension, sling operation, urethral bulking agents or even an artificial sphincter, (usually recommended for men).
For urge incontinence
Botulinum toxin, sacral nerve stimulation, posterior tibial nerve stimulation, techniques to enlarge the bladder, urinary diversion or catheterisation.
Note that, following a range of problems, mesh treatment is not currently offered within the NHS.
What can I do to get myself better now and in the future?
See a GP if you have any type of urinary incontinence. People very often self manage their bladder problems without seeking help, assuming nothing can be done. Make use of the services and professional advice that is available by first contacting your surgery.
It is important to know that urinary incontinence, which is often difficult to talk about, is not an inevitable consequence of ageing and there is a wide choice of treatments, products and management options available to people.
You should not reduce your fluids to prevent yourself passing urine.
Lifestyle changes
There are many lifestyle changes that can help to improve bladder problems in adults. These include:
• Losing weight
• Healthy diet and fluids including a reduction in caffeine
• Reducing or stopping cigarette smoking
Many people try the conservative treatments listed above. These are best discussed with your GP in case there is more that can be done to help you.
When should I seek medical attention?
See your GP if you have any type of incontinence, particularly if it affects your life in any way.
When to contact a GP quickly (“Red flags”)
• If you suddenly become incontinent
• If your bladder feels full even after you urinate
• If you have difficulty urinating when your bladder feels full
• If there is blood in your urine
Contact your GP practice, call NHS111 (if in England or Wales, NHS24 if in Scotland or Pharmacy First if in Northern Ireland) or speak to a member of your pharmacy team if you have any of these symptoms, which may indicate that you have a urine infection:
• If you feel burning or pain while urinating
• If you are urinating frequently, but only passing small amounts of urine.
• If your urine has an unusual smell
Where can I find out more?
- Expert Self Care – CONfidence App (free to download and provides help and support for people with bowel and bladder leakage (incontinence))
- Bladder and Bowel UK
- NICE
- Hartmann Advice Centre
- NHS website
- NHS Inform Scotland
- NI Direct, NI
- NHS111, Wales
We review our health information every two years and this information is due to be updated in October 2026.